Know 6 Common Skin Complications That Happen Due To Diabetes
Diabetes, one of the fastest-growing chronic diseases, affects many parts of our body, including the skin. In fact, certain changes in your skin can sometimes be the first indicator that you have diabetes.
Keep reading to know about 6 skin conditions that mostly affect people with diabetes, and also discover some helpful tips to manage them. Read on…
1. Extremely Dry, Itchy Skin
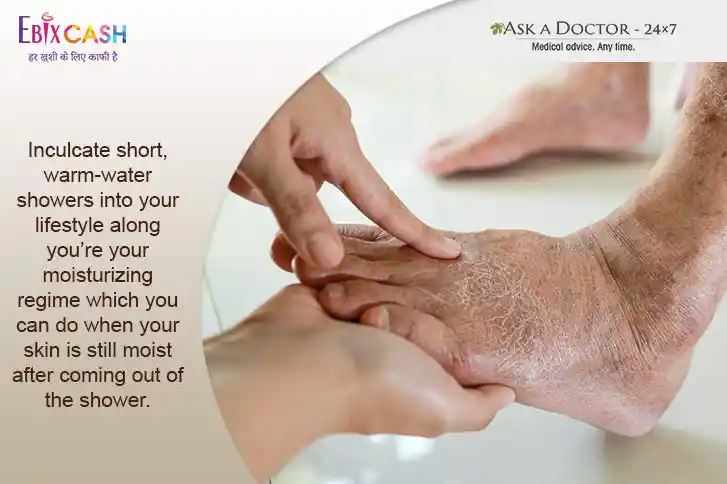
Although it is common among people who don’t have diabetes, dry, itchy skin can be a result of poor circulation, which mostly happens when you have diabetes.
Microvasculature health in the skin is very important for optimal sweat and sebaceous secretions. These secretions maintain the required moisture in the skin. In diabetes, due to poor health of vessels, improper circulation happens and both, sweat and sebaceous secretions get affected thus leading to dryness in the skin. This dryness can lead to itching without any obvious lesions.
Also, high sugar content in the blood causes the body to pull fluid from its cells so that it can produce enough urine to remove the excess sugar. This too leads to dryness in the skin.
What you can do: Monitor your blood sugar levels and keep them in control. Limit your time in the shower, use mild soaps, and make sure to apply some lotion after showering. Those with shea butter or aloe vera work better than a basic moisturizer/lotion.
Lastly, getting some exercise is one of the best ways to improve circulation—and has many health benefits.
2. Itchy rashes surrounded by tiny red blisters and scales (Fungal Infection)
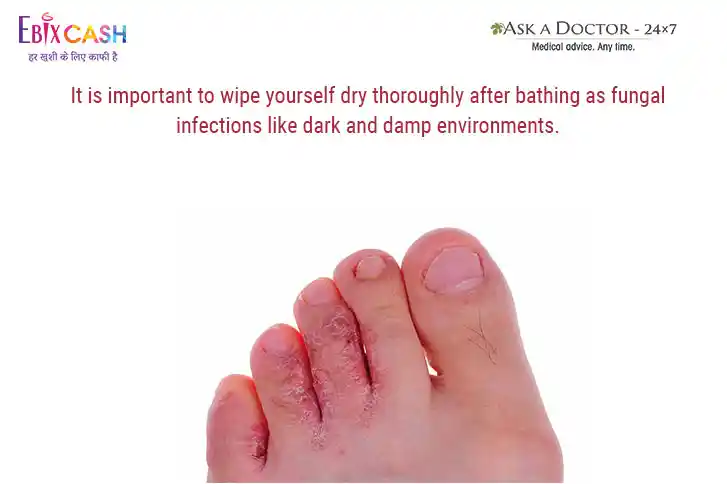
The sweat and sebaceous secretions both help in maintaining the skin’s moisture which when lost can make the skin crack, exposing micro raw areas that can be easily attacked by fungus and bacteria. Due to vascular damage in the upper layers of the skin, defenses like temperature maintenance fails which adds to the growth of infections. Some of the common fungal infections include jock itch, athlete’s foot, ringworm, and vaginal infections.
Though anyone can get a fungal infection, they are more likely to occur when blood sugar levels are high.
What you can do: Monitor your blood glucose regularly and try maintaining your numbers within the normal range. Eat low glycemic index food and get at lease 30 minutes of regular exercise 5 days a week to prevent fungal infections due to diabetes.
3. Dark patch or band of velvety skin (Acanthosis Nigricans)
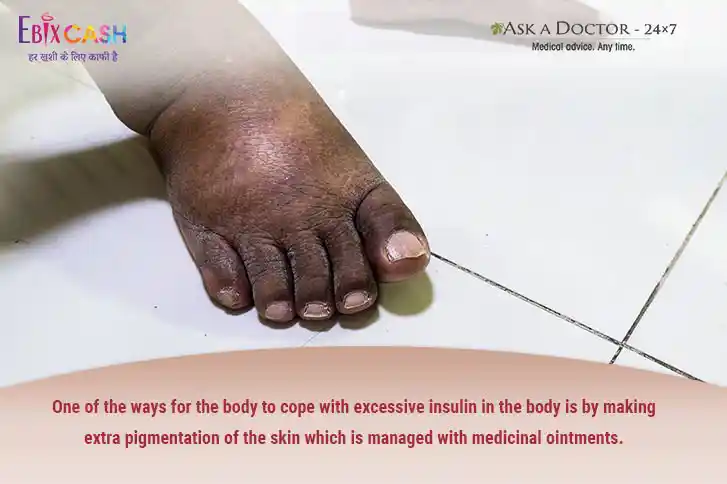
Characterized by large patches or diffuse velvety skin more commonly seen behind the neck, at the armpits, elbows, groin etc., these patches do not itch or hurt.
This occurs mostly due to the pathology of diabetes itself rather than its complication. The appearance of such patches indicates increased levels of non-functional insulin in the body, which can be seen in type 2 diabetes and even in people with prediabetes. Therefore, sometimes it is considered a marker for diabetes.
What you can do: No sooner you observe acanthosis must go for diabetes screening at the earliest. There is no specific treatment for this condition although it can fade off with decreasing insulin resistance by weight loss and lifestyle changes.
4. Brownish Round to Stellar Patches or Lines within the skin (Diabetic Dermopathy)
One of the most common cosmetic skin condition, such patches mainly occurs on the limbs, and is not associated with pain or itching. Usually, these start from the ankles and wrists and spread over the entire limb over years.
What you can do: They do not respond to any treatment. The patches appear in proportion to high glucose levels. Better glycemic control can lead to the avoidance of the new emergence of diabetic dermopathy.
5. Small, Raised Bumps that Turns into Yellow Hard Patches (Necrobiosis Lipoidica Diabeticorum)
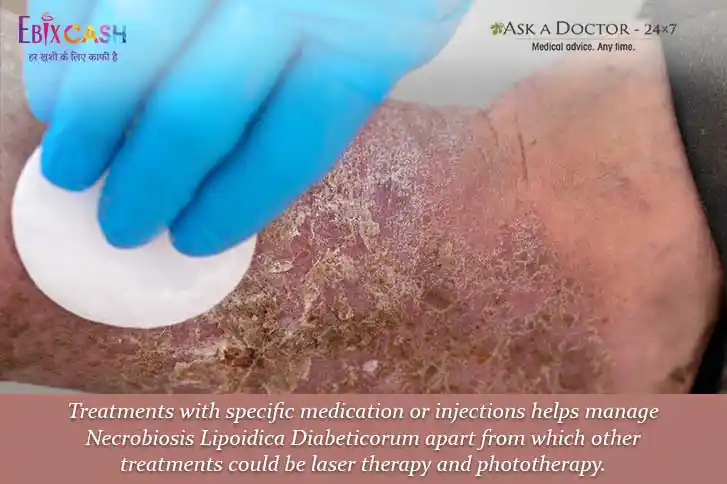
Although similar to the patches seen in diabetic dermopathy, Necrobiosis Lipoidica Diabeticorum are bigger and fewer in number. They harbor a mild amount of inflammation owing to their depth into the skin layers, exposing the underlying areas which show intense immune response to the external environment.
This reaction in the lesion makes them itchy and sometimes painful.
What you can do: Seek medical advice or your doctors, ASAP. Antibiotics and anti-inflammatory medications can reduce inflammation and provide relief from itching and pain caused by these patches.
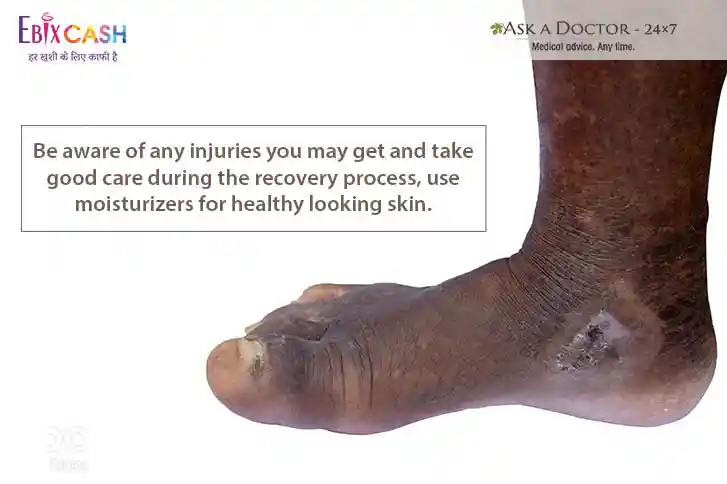
6. Diabetic Blisters (Bullous Diabeticorum)
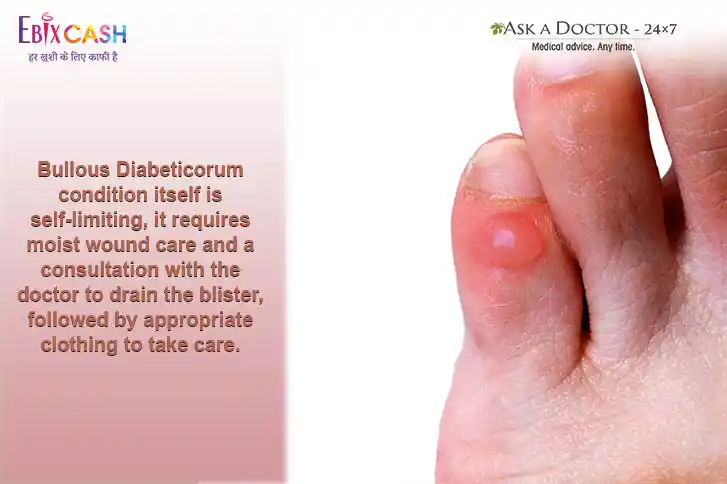
These rare but serious skin lesions suddenly appear on the skin of people with diabetes. Very often these are seen on the hands, feet, legs, or forearms and look like fluid-filled blisters that appear after a serious burn. These blebs are very fragile and break open leaving raw surfaces which can get infected. However, unlike burn blisters are not painful.
What you can do: Take help from a diabetologist or your doctor to better control your diabetes. Also, eat mindfully to avoid all high glycemic index foods, and stay active.
Skincare is a very important in diabetics as these infections can extend to any organ or muscle beneath and can cause serious life-threatening problems. Imbibe good habits by regularly moisturizing your overall skin, avoiding scratching, going for routine foot examinations, and strictly adhering to diabetes control. Stay aware and mindful to keep diabetes as well as skin problems away.
Have some other queries related to skincare and diabetes? You can consult our Endocrinologist or Derma Specialist to seek medical advice, anytime.
Ask a Specialist
Recent Questions


